Corneal Transplant
The cornea is the front, outermost layer of the eye. Just as a window lets light into a room, the cornea lets light into the eye. It also focuses the light passing through it to make images clear and sharp.
Corneal problems can happen to anyone at any age. Sometimes due to disease, injury or infection the cornea becomes cloudy or warped. A damaged cornea, like a frosted or misshapen windowpane, distorts light as it enters the eye. This causes distortion in vision.
When there is no other remedy, doctors advise a corneal transplant. In this procedure an ophthalmologist surgically replaces the diseased cornea with a healthy one to restore clear vision.
This leaflet will answer some questions that you may have about corneal transplants.
How does the eye work?
Anything you see is an image that enters your eye in the form of light. The different parts of your eye collect this light and send a message to your brain, enabling you to see. For perfect vision all the parts of your eye need to work properly.
What is a corneal transplant?
The corneal tissue used for transplantation is supplied by an Eye Bank. Eye Banks work round the clock to collect, evaluate, and store donated corneas. The corneas are collected from human donors within hours of death. Stringent tests are done to ensure the safety of the person receiving the cornea. The Eye Bank verifies the donor's medical history and cause of death, and performs blood tests to ensure that the deceased person did not have any contagious disease, such as AlDS or hepatitis.
Light rays passing through a healthy cornea
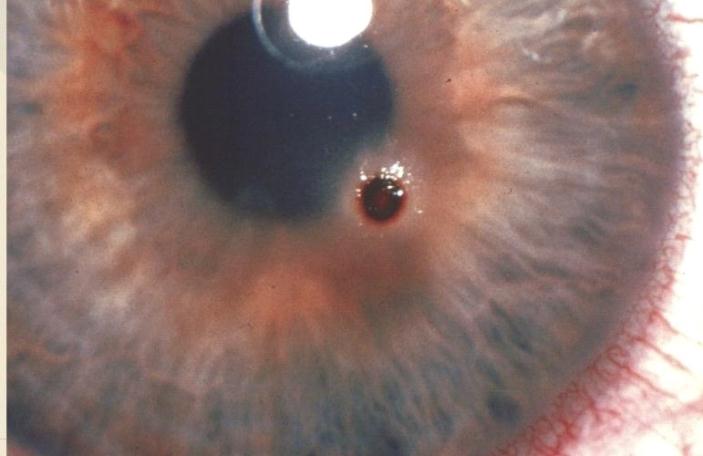
- The cornea is the clear, outer layer of the eye.
- The pupil isan openingthat lets light enterthe eye.
- The iris, the colored part of the eye, makes the pupil larger or smaller.
- The lens bends to focus light onto the retina.
- The retina receives light that has been focused by the cornea and lens.
A clear(vitreous)gel fills the inside of the eye, giving it shape.
The cornea is clear so as to let light into the eye, and curved to focus the light rays onto the retina, through the lens.
Before the procedure
- It is not necessary to find a cornea with a matching tissue or blood type
- The race, gender, and eye color of the donor are not important
- A corneal transplant won't change your natural eye color
- The cornea heals slowly and improvement in vision may take a year or more
- It is difficult to shape the new cornea perfectly. So astigmatism (a condition where the cornea has an irregular shape, making images seem blurred or distorted) is common aftera corneal transplant
- However, this can be corrected with glasses
Scheduling a transplant
If you are advised to undergo a corneal transplant, your ophthalmologist will tell you about the procedure. The transplant will be scheduled according to the condition of your eye and availability of a donor cornea. Sometimes shortage of donor corneas may delay surgery.
If both your eyes need new corneas, the second transplant will not be performed until the first eye has stabilized, which may take up to a year.
Preparing for surgery
If you are taking any other medication, ask your ophthalmologist whetheryou should continue it. You will probably be asked not to eat or drink anything for several hours before the surgery.
Usually local anesthesia is used, so you will be awake but feel no pain. The nerves in your eye will be completely numbed so you will not be able to see or move your eye. Sometimes the doctor may use general anesthesia.
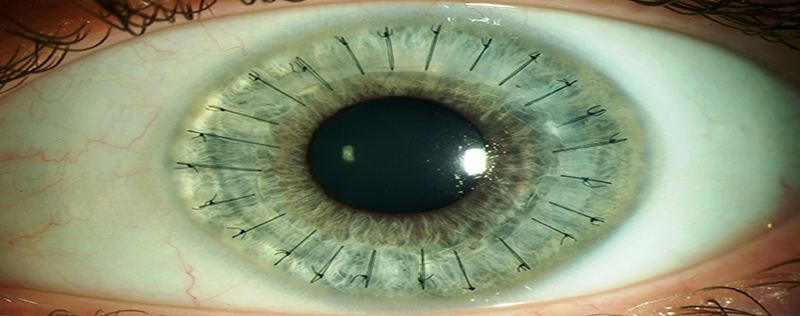
The transplant procedure
For the transplant, doctors use an operating microscope and very delicate instruments. Once the old cornea is removed, the new cornea is stitched into place. The sutures or stitches are barely visible and are not painful, although you may feel some irritation ora scratching sensation for a few days.
If necessary, other procedures, may be performed at the same time as your transplant. Your ophthalmologist will advise you about them.
Potential risks
As with other surgical procedures, a corneal transplant involves some risks and most of them can be treated. Some possible complications are:
- Eye infections
- Failure of the donor cornea to function normally
- Rejection of the donor cornea by your body
- Cataract(clouding of the eye's lens)
- Glaucoma (build-up of fluid, leading to increased pressure in the eye)
- Bleeding from the iris
- Swelling or detachment of the retina
Rejection: The danger signals!
Rejection of a transplanted cornea can occur any time, but is more likely to happen in the first year after surgery. Rejection reduces the chance of success of any repeat corneal transplantation. However, rejection can be prevented by good compliance with post op medication, timely diagnosis and appropriate management.
Watch out for these danger signals:
Redness
Sensitivity to light
Vision loss
Pain
The acronym 'RSVP' can help you remember these symptoms. If you notice any of these in your operated eye, however minor they may seem and regardless of the time of day, contact us immediately. If this is not possible, visit an ophthalmologist, preferably a cornea specialist.
Care after surgery
- Do not lift heavy things
- Do not bend so that your head is lower than your waist
- Avoid sleeping on the operated side for a few days
- No sexual intercourse until permitted by the doctor
- Do not rub the operated eye
- Avoid any vigorous activity
- Avoid alcoholic beverages
- Watch television only for short periods
You can bathe carefully from below the neck and shave, but do not let the operated eye get wet for at least 15 days. You may gently clean the eyelids with a piece of cotton boiled in water or a sterilized tissue. Do not wet the eyeball. You should wear an eye patch at night; the doctor willadvise you when to discontinue using it during the day. Always wear protective glasses or an 'eye shield' to avoid accidental injury.
Medication and follow-up
At the time of discharge our patient counselor will advise you about medication and follow-up visits. Please follow the instructions regarding medication. Please adhere to the follow up appointment date.
If you have any concerns or questions, ask the doctor when you come for an examination. If you feel you cannot wait, call or email us.
If there is an emergency at night, during a weekend, or on a holiday, visit your nearest hospital.
Always mention the patient's ID number, name and the doctor's name in all communications.